Stroke is the fifth leading cause of death in the United States and is a major cause of adult disability. About 800,000 people in the United States have a stroke each year. One American dies from a stroke, on average, every 4 minutes. [From: stroke facts]
A stroke occurs if the flow of oxygen-rich blood to a portion of the brain is blocked. Without oxygen, brain cells start to die after a few minutes. Sudden bleeding in the brain also can cause a stroke if it damages brain cells.
If brain cells die or are damaged because of a stroke, symptoms occur in the parts of the body that these brain cells control. Examples of stroke symptoms include sudden weakness; paralysis or numbness of the face, arms, or legs (paralysis is an inability to move); trouble speaking or understanding speech; and trouble seeing.
A stroke is a serious medical condition that requires emergency care. A stroke can cause lasting brain damage, long-term disability, or even death.
If you think you or someone else is having a stroke, call 9–1–1 right away. Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room. During a stroke, every minute counts.
Overview
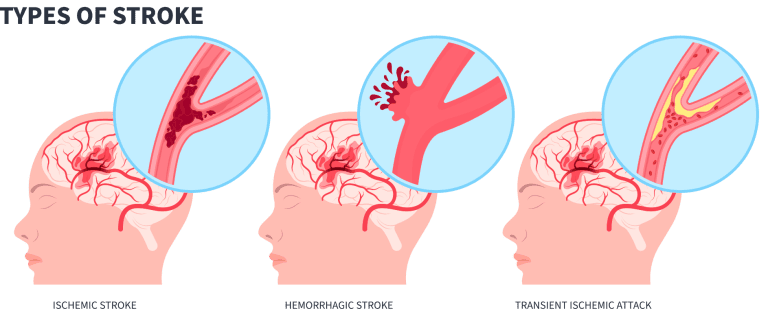
The two main types of stroke are ischemic (is-KE-mik) and hemorrhagic (hem-ah-RAJ-ik). Ischemic is the more common type of stroke.
An ischemic stroke occurs if an artery that supplies oxygen-rich blood to the brain becomes blocked. Blood clots often cause the blockages that lead to ischemic strokes.
A hemorrhagic stroke occurs if an artery in the brain leaks blood or ruptures (breaks open). The pressure from the leaked blood damages brain cells. High blood pressure and aneurysms (AN-u-risms) are examples of conditions that can cause hemorrhagic strokes. (Aneurysms are balloon-like bulges in an artery that can stretch and burst.)
Another condition that’s similar to a stroke is a transient ischemic attack, also called a TIA or “mini-stroke.” A TIA occurs if blood flow to a portion of the brain is blocked only for a short time. Thus, damage to the brain cells isn’t permanent (lasting).
Like ischemic strokes, TIAs often are caused by blood clots. Although TIAs are not full-blown strokes, they greatly increase the risk of having a stroke. If you have a TIA, it’s important for your doctor to find the cause so you can take steps to prevent a stroke.
Both strokes and TIAs require emergency care.
Outlook
Stroke is a leading cause of death in the United States. Many factors can raise your risk of having a stroke. Talk with your doctor about how you can control these risk factors and help prevent a stroke.
If you have a stroke, prompt treatment can reduce damage to your brain and help you avoid lasting disabilities. Prompt treatment also may help prevent another stroke.
Researchers continue to study the causes and risk factors for stroke. They’re also finding new and better treatments and new ways to help the brain repair itself after a stroke.
Source: National Institutes of Health
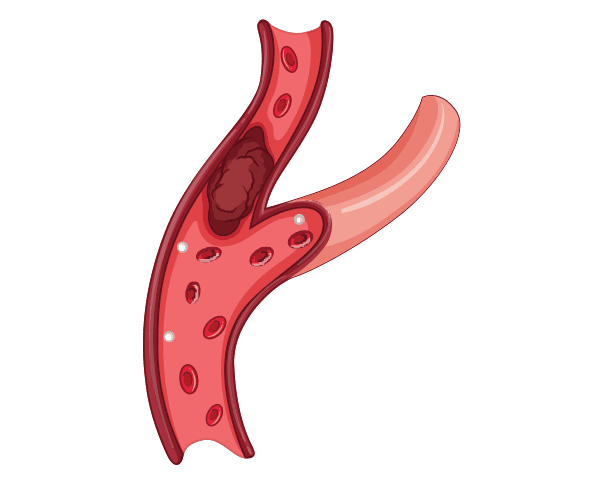
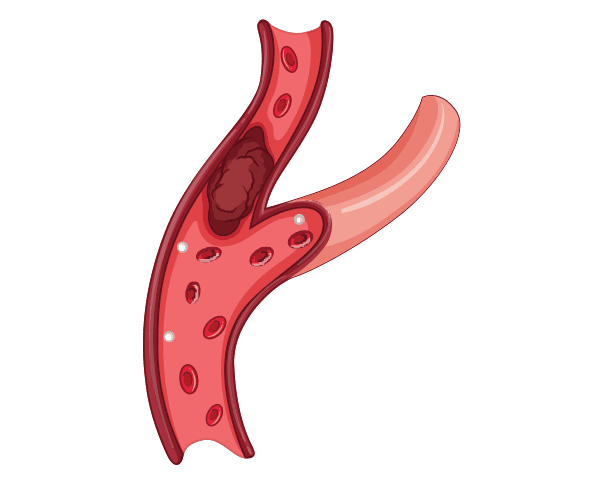
An ischemic stroke occurs if an artery that supplies oxygen-rich blood to the brain becomes blocked. Blood clots often cause the blockages that lead to ischemic strokes.
The two types of ischemic stroke are thrombotic (throm-BOT-ik) and embolic (em-BOL-ik). In a thrombotic stroke, a blood clot (thrombus) forms in an artery that supplies blood to the brain.
In an embolic stroke, a blood clot or other substance (such as plaque, a fatty material) travels through the bloodstream to an artery in the brain. (A blood clot or piece of plaque that travels through the bloodstream is called an embolus.)
With both types of ischemic stroke, the blood clot or plaque blocks the flow of oxygen-rich blood to a portion of the brain.
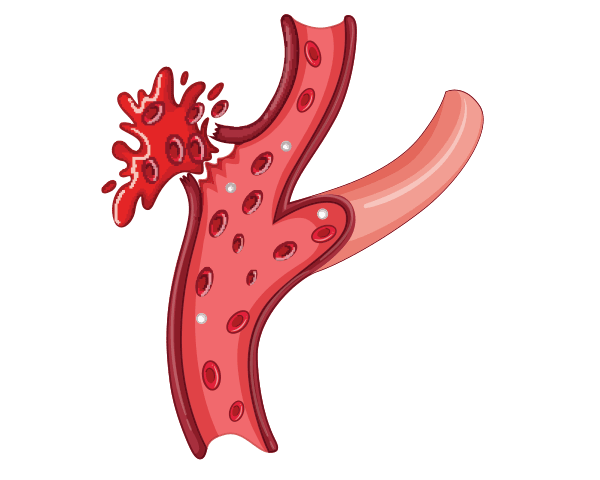
A hemorrhagic stroke occurs if an artery in the brain leaks blood or ruptures (breaks open). The pressure from the leaked blood damages brain cells.
The two types of hemorrhagic stroke are intracerebral (in-trah-SER-e-bral) and subarachnoid (sub-ah-RAK-noyd). In an intracerebral hemorrhage, a blood vessel inside the brain leaks blood or ruptures.
In a subarachnoid hemorrhage, a blood vessel on the surface of the brain leaks blood or ruptures. When this happens, bleeding occurs between the inner and middle layers of the membranes that cover the brain.
In both types of hemorrhagic stroke, the leaked blood causes swelling of the brain and increased pressure in the skull. The swelling and pressure damage cells and tissues in the brain.
Source: National Institutes of Health
A transient ischemic attack sometimes is called a TIA or mini-stroke. A TIA has the same symptoms as a stroke, and it increases your risk of having a stroke.
Source: National Institutes of Health
Ischemic Stroke and Transient Ischemic Attack
An ischemic stroke or transient ischemic attack (TIA) occurs if an artery that supplies oxygen-rich blood to the brain becomes blocked. Many medical conditions can increase the risk of ischemic stroke or TIA.
For example, atherosclerosis (ath-er-o-skler-O-sis) is a disease in which a fatty substance called plaque builds up on the inner walls of the arteries. Plaque hardens and narrows the arteries, which limits the flow of blood to tissues and organs (such as the heart and brain).

Plaque in an artery can crack or rupture (break open). Blood platelets (PLATE-lets), which are disc-shaped cell fragments, stick to the site of the plaque injury and clump together to form blood clots. These clots can partly or fully block an artery.
Plaque can build up in any artery in the body, including arteries in the heart, brain, and neck. The two main arteries on each side of the neck are called the carotid (ka-ROT-id) arteries. These arteries supply oxygen-rich blood to the brain, face, scalp, and neck.
When plaque builds up in the carotid arteries, the condition is called carotid artery disease. Carotid artery disease causes many of the ischemic strokes and TIAs that occur in the United States.
An embolic stroke (a type of ischemic stroke) or TIA also can occur if a blood clot or piece of plaque breaks away from the wall of an artery. The clot or plaque can travel through the bloodstream and get stuck in one of the brain’s arteries. This stops blood flow through the artery and damages brain cells.
Heart conditions and blood disorders also can cause blood clots that can lead to a stroke or TIA. For example, atrial fibrillation (A-tre-al fi-bri-LA-shun), or AF, is a common cause of embolic stroke.
In AF, the upper chambers of the heart contract in a very fast and irregular way. As a result, some blood pools in the heart. The pooling increases the risk of blood clots forming in the heart chambers.
An ischemic stroke or TIA also can occur because of lesions caused by atherosclerosis. These lesions may form in the small arteries of the brain, and they can block blood flow to the brain.
Hemorrhagic Stroke
Sudden bleeding in the brain can cause a hemorrhagic stroke. The bleeding causes swelling of the brain and increased pressure in the skull. The swelling and pressure damage brain cells and tissues.
Examples of conditions that can cause a hemorrhagic stroke include high blood pressure, aneurysms, and arteriovenous (ar-TEER-e-o-VE-nus) malformations (AVMs).
"Blood pressure" is the force of blood pushing against the walls of the arteries as the heart pumps blood. If blood pressure rises and stays high over time, it can damage the body in many ways.
Aneurysms are balloon-like bulges in an artery that can stretch and burst. AVMs are tangles of faulty arteries and veins that can rupture within the brain. High blood pressure can increase the risk of hemorrhagic stroke in people who have aneurysms or AVMs.
Source: National Institutes of Health
Certain traits, conditions, and habits can raise your risk of having a stroke or transient ischemic attack (TIA). These traits, conditions, and habits are known as risk factors. The more risk factors you have, the more likely you are to have a stroke. You can treat or control some risk factors, such as high blood pressure and smoking. Other risk factors, such as age and gender, you can’t control.
The major risk factors for stroke include:
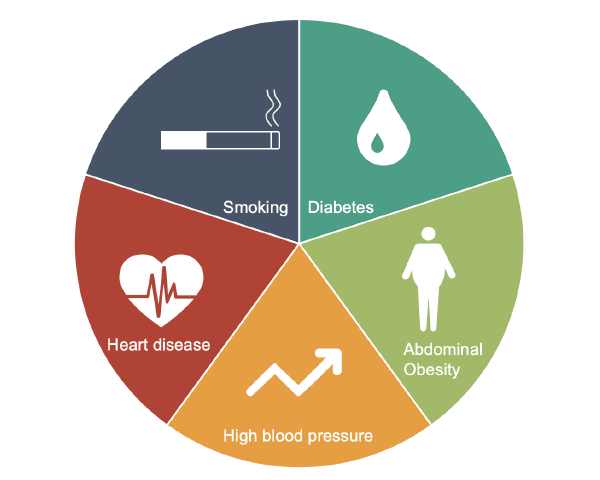
Other risk factors for stroke, many of which of you can control, include:
Following a healthy lifestyle can lower the risk of stroke. Some people also may need to take medicines to lower their risk.
Sometimes strokes can occur in people who don’t have any known risk factors.
Source: National Institutes of Health
The signs and symptoms of a stroke often develop quickly. However, they can develop over hours or even days.
The type of symptoms depends on the type of stroke and the area of the brain that’s affected. How long symptoms last and how severe they are vary among different people.
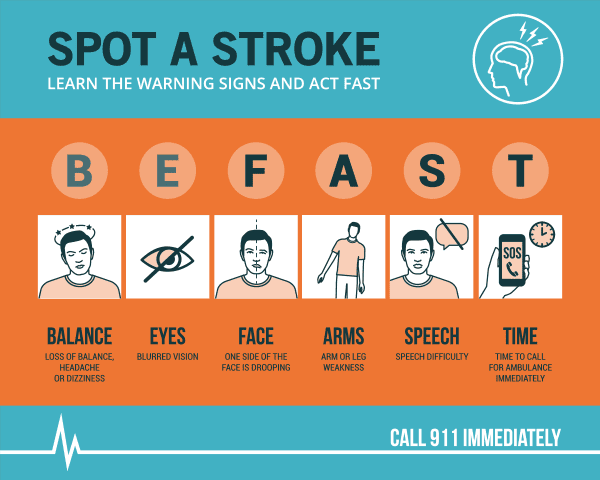
Signs and symptoms of a stroke may include:
A transient ischemic attack (TIA) has the same signs and symptoms as a stroke. However, TIA symptoms usually last less than 1–2 hours (although they may last up to 24 hours). A TIA may occur only once in a person’s lifetime or more often.
At first, it may not be possible to tell whether someone is having a TIA or stroke. All stroke-like symptoms require medical care.
If you think you or someone else is having a TIA or stroke, call 9–1–1 right away. Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room. During a stroke, every minute counts.
Stroke Complications
After you’ve had a stroke, you may develop other complications, such as:
Additional: Stroke Warning Signs and Symptoms
Source: National Institutes of Health
Your doctor will diagnose a stroke based on your signs and symptoms, your medical history, a physical exam, and test results.
Your doctor will want to find out the type of stroke you’ve had, its cause, the part of the brain that's affected, and whether you have bleeding in the brain.
If your doctor thinks you’ve had a transient ischemic attack (TIA), he or she will look for its cause to help prevent a future stroke.
Medical History and Physical Exam
Your doctor will ask you or a family member about your risk factors for stroke. Examples of risk factors include high blood pressure, smoking, heart disease, and a personal or family history of stroke. Your doctor also will ask about your signs and symptoms and when they began.
During the physical exam, your doctor will check your mental alertness and your coordination and balance. He or she will check for numbness or weakness in your face, arms, and legs; confusion; and trouble speaking and seeing clearly.
Your doctor will look for signs of carotid artery disease, a common cause of ischemic stroke. He or she will listen to your carotid arteries with a stethoscope. A whooshing sound called a bruit (broo-E) may suggest changed or reduced blood flow due to plaque buildup in the carotid arteries.
Diagnostic Tests and Procedures
Your doctor may recommend one or more of the following tests to diagnose a stroke or TIA.
Brain Computed Tomography
A brain computed tomography (to-MOG-rah-fee) scan, or brain CT scan, is a painless test that uses x rays to take clear, detailed pictures of your brain. This test often is done right after a stroke is suspected.
A brain CT scan can show bleeding in the brain or damage to the brain cells from a stroke. The test also can show other brain conditions that may be causing your symptoms.
Magnetic Resonance Imaging
Magnetic resonance imaging (MRI) uses magnets and radio waves to create pictures of the organs and structures in your body. This test can detect changes in brain tissue and damage to brain cells from a stroke.
An MRI may be used instead of, or in addition to, a CT scan to diagnose a stroke.
Computed Tomography Arteriogram and Magnetic Resonance Arteriogram
A CT arteriogram (CTA) and magnetic resonance arteriogram (MRA) can show the large blood vessels in the brain. These tests may give your doctor more information about the site of a blood clot and the flow of blood through your brain.
Carotid Ultrasound
Carotid ultrasound is a painless and harmless test that uses sound waves to create pictures of the insides of your carotid arteries. These arteries supply oxygen-rich blood to your brain.
Carotid ultrasound shows whether plaque has narrowed or blocked your carotid arteries.
Your carotid ultrasound test may include a Doppler ultrasound. Doppler ultrasound is a special test that shows the speed and direction of blood moving through your blood vessels.
Carotid Angiography
Carotid angiography (an-jee-OG-ra-fee) is a test that uses dye and special x rays to show the insides of your carotid arteries.
For this test, a small tube called a catheter is put into an artery, usually in the groin (upper thigh). The tube is then moved up into one of your carotid arteries.
Your doctor will inject a substance (called contrast dye) into the carotid artery. The dye helps make the artery visible on x-ray pictures.
Heart Tests
EKG (Electrocardiogram)
An EKG is a simple, painless test that records the heart's electrical activity. The test shows how fast the heart is beating and its rhythm (steady or irregular). An EKG also records the strength and timing of electrical signals as they pass through each part of the heart.
An EKG can help detect heart problems that may have led to a stroke. For example, the test can help diagnose atrial fibrillation or a previous heart attack.
Echocardiography
Echocardiography (EK-o-kar-de-OG-ra-fee), or echo, is a painless test that uses sound waves to create pictures of your heart.
The test gives information about the size and shape of your heart and how well your heart's chambers and valves are working.
Echo can detect possible blood clots inside the heart and problems with the aorta. The aorta is the main artery that carries oxygen-rich blood from your heart to all parts of your body.
Blood Tests
Your doctor also may use blood tests to help diagnose a stroke.
A blood glucose test measures the amount of glucose (sugar) in your blood. Low blood glucose levels may cause symptoms similar to those of a stroke.
A platelet count measures the number of platelets in your blood. Blood platelets are cell fragments that help your blood clot. Abnormal platelet levels may be a sign of a bleeding disorder (not enough clotting) or a thrombotic disorder (too much clotting).
Your doctor also may recommend blood tests to measure how long it takes for your blood to clot. Two tests that may be used are called PT and PTT tests. These tests show whether your blood is clotting normally.
Source: National Institutes of Health
Treatment for a stroke depends on whether it is ischemic or hemorrhagic. Treatment for a transient ischemic attack (TIA) depends on its cause, how much time has passed since symptoms began, and whether you have other medical conditions.
Strokes and TIAs are medical emergencies. If you have stroke symptoms, call 9–1–1 right away. Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room. During a stroke, every minute counts.
Once you receive initial treatment, your doctor will try to treat your stroke risk factors and prevent complications.
Treating Ischemic Stroke and Transient Ischemic Attack
An ischemic stroke or TIA occurs if an artery that supplies oxygen-rich blood to the brain becomes blocked. Often, blood clots cause the blockages that lead to ischemic strokes and TIAs.
Treatment for an ischemic stroke or TIA may include medicines and medical procedures.
Medicines
A medicine called tissue plasminogen activator (tPA) can break up blood clots in the arteries of the brain. A doctor will inject tPA into a vein in your arm. This medicine must be given within 4 hours of the start of symptoms to work. Ideally, it should be given as soon as possible.
If, for medical reasons, your doctor can’t give you tPA, you may get an antiplatelet medicine. For example, aspirin may be given within 48 hours of a stroke. Antiplatelet medicines help stop platelets from clumping together to form blood clots.
Your doctor also may prescribe anticoagulants, or “blood thinners.” These medicines can keep blood clots from getting larger and prevent new blood clots from forming.
Medical Procedures
If you have carotid artery disease, your doctor may recommend a carotid endarterectomy (END-ar-ter-EK-to-me) or carotid artery percutaneous (per-ku-TA-ne-us) coronary intervention, sometimes referred to as angioplasty (AN-jee-oh-plas-tee). Both procedures open blocked carotid arteries.
Researchers are testing other treatments for ischemic stroke, such as intra-arterial thrombolysis (throm-BOL-ih-sis) and mechanical clot (embolus) removal in cerebral ischemia (MERCI).
In intra-arterial thrombolysis, a long flexible tube called a catheter is put into your groin (upper thigh) and threaded to the tiny arteries of the brain. Your doctor can deliver medicine through this catheter to break up a blood clot in the brain.
MERCI is a device that can remove blood clots from an artery. During the procedure, a catheter is threaded through a carotid artery to the affected artery in the brain. The device is then used to pull the blood clot out through the catheter.
Treating Hemorrhagic Stroke
A hemorrhagic stroke occurs if an artery in the brain leaks blood or ruptures (breaks open). The first steps in treating a hemorrhagic stroke are to find the cause of bleeding in the brain and then control it.
Unlike ischemic strokes, hemorrhagic strokes aren’t treated with antiplatelet medicines and blood thinners. This is because these medicines can make bleeding worse.
If you’re taking antiplatelet medicines or blood thinners and have a hemorrhagic stroke, you’ll be taken off the medicine.
If high blood pressure is the cause of bleeding in the brain, your doctor may prescribe medicines to lower your blood pressure. This can help prevent further bleeding.
Surgery also may be needed to treat a hemorrhagic stroke. The types of surgery used include aneurysm clipping, coil embolization (EM-bol-ih-ZA-shun), and arteriovenous malformation (AVM) repair.
Aneurysm Clipping and Coil Embolization
If an aneurysm (a balloon-like bulge in an artery) is the cause of a stroke, your doctor may recommend aneurysm clipping or coil embolization.
Aneurysm clipping is done to block off the aneurysm from the blood vessels in the brain. This surgery helps prevent further leaking of blood from the aneurysm. It also can help prevent the aneurysm from bursting again.
During the procedure, a surgeon will make an incision (cut) in the brain and place a tiny clamp at the base of the aneurysm. You’ll be given medicine to make you sleep during the surgery. After the surgery, you’ll need to stay in the hospital’s intensive care unit for a few days.
Coil embolization is a less complex procedure for treating an aneurysm. The surgeon will insert a tube called a catheter into an artery in the groin. He or she will thread the tube to the site of the aneurysm.
Then, a tiny coil will be pushed through the tube and into the aneurysm. The coil will cause a blood clot to form, which will block blood flow through the aneurysm and prevent it from bursting again.
Coil embolization is done in a hospital. You’ll be given medicine to make you sleep during the surgery.
Arteriovenous Malformation Repair
If an AVM is the cause of a stroke, your doctor may recommend an AVM repair. (An AVM is a tangle of faulty arteries and veins that can rupture within the brain.) AVM repair helps prevent further bleeding in the brain.
Doctors use several methods to repair AVMs. These methods include:
Surgery to remove the AVM
Injecting a substance into the blood vessels of the AVM to block blood flow
Using radiation to shrink the blood vessels of the AVM
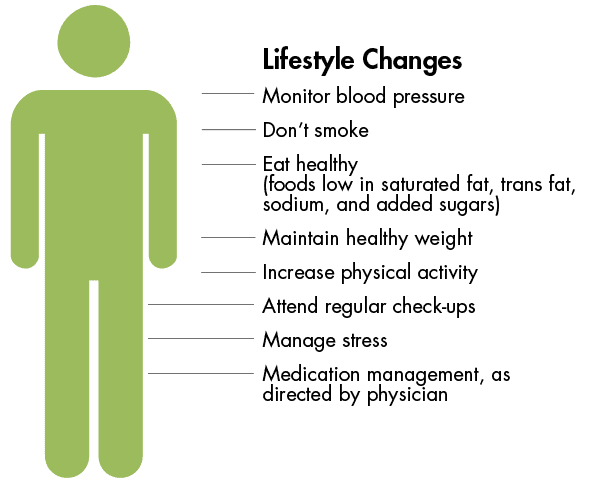
Treating Stroke Risk Factors
After initial treatment for a stroke or TIA, your doctor will treat your risk factors. He or she may recommend lifestyle changes to help control your risk factors.
Lifestyle changes may include quitting smoking, following a healthy diet, maintaining a healthy weight, and being physically active.
If lifestyle changes aren’t enough, you may need medicine to control your risk factors.
Following a Healthy Diet
A healthy diet is an important part of a healthy lifestyle. Choose a variety of fruits, vegetables, and grains; half of your grains should come from whole-grain products.
Choose foods that are low in saturated fat, trans fat, and cholesterol. Healthy choices include lean meats, poultry without skin, fish, beans, and fat-free or low-fat milk and milk products.
Choose and prepare foods with little sodium (salt). Too much salt can raise your risk of high blood pressure. Studies show that following the Dietary Approaches to Stop Hypertension (DASH) eating plan can lower blood pressure.
Choose foods and beverages that are low in added sugar. If you drink alcoholic beverages, do so in moderation.
For more information about following a healthy diet, go to the NHLBI’s Aim for a Healthy Weight Web site, “Your Guide to a Healthy Heart,” and “Your Guide to Lowering Your Blood Pressure With DASH.” All of these resources provide general information about healthy eating.
Quitting Smoking
If you smoke or use tobacco, quit. Smoking can damage your blood vessels and raise your risk of stroke and other health problems. Talk with your doctor about programs and products that can help you quit. Also, try to avoid secondhand smoke. Secondhand smoke also can damage the blood vessels.
For more information about how to quit smoking, go to the Health Topics Smoking and Your Heart article and the National Heart, Lung, and Blood Institute’s (NHLBI’s) "Your Guide to a Healthy Heart." Although these resources focus on heart health, they include general information about how to quit smoking.
The U.S. Department of Health and Human Services (HHS) also has information about how to quit smoking.
Maintaining a Healthy Weight
Maintaining a healthy weight can lower your risk of stroke. A general goal to aim for is a body mass index (BMI) of less than 25.
BMI measures your weight in relation to your height and gives an estimate of your total body fat. You can measure your BMI using the NHLBI's online calculatorexternal link icon, or your health care provider can measure your BMI.
A BMI between 25 and 29.9 is considered overweight. A BMI of 30 or more is considered obese. A BMI of less than 25 is the goal for preventing a stroke.
For more information about losing weight and maintaining your weight, go to the HEALTH TOPICS Overweight and Obesity article.
Being Physically Active
Regular physical activity can help control many stroke risk factors, such as high blood pressure, unhealthy cholesterol levels, and excess weight.
Talk with your doctor before you start a new exercise plan. Ask him or her how much and what kinds of physical activity are safe for you.
People gain health benefits from as little as 60 minutes of moderate-intensity aerobic activity per week. The more active you are, the more you will benefit.
For more information about physical activity, go to the HHS’ "2008 Physical Activity Guidelines for Americans,"external link icon the HEALTH TOPICS Physical Activity and Your Heart article, and the NHLBI's "Your Guide to Physical Activity and Your Heart."
Although the HEALTH TOPICS article and “Your Guide” booklet focus on heart health, they include information that applies to general health and well-being.
Additional: Stroke Treatment
Source: National Institutes of Health
Taking action to control your risk factors can help prevent or delay a stroke. If you’ve already had a stroke, these actions can help prevent another one.
For more information about healthy lifestyle changes, go to “How Is a Stroke Treated?” If lifestyle changes are not enough, you also may need medicines to control your stroke risk factors. Take all of your medicines as your doctor prescribes.
If you’ve had a transient ischemic attack (TIA), don’t ignore it. It’s important for your doctor to find the cause of the TIA so you can take steps to prevent a stroke.
Additional: Understanding Stroke Risk
Source: National Institutes of Health
The time it takes to recover from a stroke varies—it can take weeks, months, or even years. Some people recover fully, while others have long-term or lifelong disabilities.
Ongoing care, rehabilitation, and emotional support can help you recover and may even help prevent another stroke.
If you’ve had a stroke, you’re at risk of having another one. Know the warning signs of a stroke and transient ischemic attack (TIA) and what to do if they occur. Call 9–1–1 as soon as symptoms start.
Do not drive to the hospital or let someone else drive you. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room. During a stroke, every minute counts.
Ongoing Care
Lifestyle changes can help you recover from a stroke and may help prevent another one. Examples of these changes include quitting smoking, following a healthy diet, maintaining a healthy weight, and being physically active. Talk with your doctor about the types and amounts of physical activity that are safe for you.
Your doctor also may prescribe medicines to help you recover from a stroke or control your stroke risk factors. Take all of your medicines as your doctor prescribes.
If you had an ischemic stroke, you may need to take anticoagulants, also called blood thinners. These medicines prevent blood clots from getting larger and keep new clots from forming. You’ll likely need routine blood tests to check how well these medicines are working.
The most common side effect of blood thinners is bleeding. This happens if the medicine thins your blood too much. This side effect can be life threatening. Bleeding can occur inside your body cavities (internal bleeding) or from the surface of your skin (external bleeding).
Know the warning signs of bleeding so you can get help right away. They include:
A lot of bleeding after a fall or injury or easy bruising or bleeding also may mean that your blood is too thin. Call your doctor right away if you have any of these signs. If you have severe bleeding, call 9–1–1.
Talk with your doctor about how often you should schedule followup visits or tests. These visits and tests can help your doctor monitor your stroke risk factors and adjust your treatment as needed.
Rehabilitation
After a stroke, you may need rehabilitation (rehab) to help you recover. Rehab may include working with speech, physical, and occupational therapists.
Language, Speech, and Memory
You may have trouble communicating after a stroke. You may not be able to find the right words, put complete sentences together, or put words together in a way that makes sense. You also may have problems with your memory and thinking clearly. These problems can be very frustrating.
Speech and language therapists can help you learn ways to communicate again and improve your memory.
Muscle and Nerve Problems
A stroke may affect only one side of the body or part of one side. It can cause paralysis (an inability to move) or muscle weakness, which can put you at risk for falling.
Physical and occupational therapists can help you strengthen and stretch your muscles. They also can help you relearn how to do daily activities, such as dressing, eating, and bathing.
Bladder and Bowel Problems
A stroke can affect the muscles and nerves that control the bladder and bowels. You may feel like you have to urinate often, even if your bladder isn’t full. You may not be able to get to the bathroom in time. Medicines and a bladder or bowel specialist can help with these problems.
Swallowing and Eating Problems
You may have trouble swallowing after a stroke. Signs of this problem are coughing or choking during eating or coughing up food after eating.
A speech therapist can help you with these issues. He or she may suggest changes to your diet, such as eating puréed (finely chopped) foods or drinking thick liquids.
Emotional Issues and Support
After a stroke, you may have changes in your behavior or judgment. For example, your mood may change quickly. Because of these and other changes, you may feel scared, anxious, and depressed. Recovering from a stroke can be slow and frustrating.
Talk about how you feel with your health care team. Talking to a professional counselor also can help. If you’re very depressed, your doctor may recommend medicines or other treatments that can improve your quality of life.
Joining a patient support group may help you adjust to life after a stroke. You can see how other people have coped with having strokes. Talk with your doctor about local support groups or check with an area medical center.
Support from family and friends also can help relieve fear and anxiety. Let your loved ones know how you feel and what they can do to help you.
Additional: Life After Stroke
Source: National Institutes of Health
Stroke is consistently one of the leading causes of death in the United, is a major cause of adult disability, and appears in a vast spectrum of people. It can be caused by substance abuse, stress, cardiac conditions, genetic abnormalities, and medical comorbidities. When treated with individualized therapies and goal-oriented programs, the effects of stroke can be overcome. CNS focuses on rebuilding life skills, helping people to walk, speak, work, reason, and function in the world again.
Find a support group near you: Stroke Support Finder
Every Brain Injury is Different (The Broad Strokes of Stroke)
From Everyday Lives: Four Real-Life Accounts of Stroke
CNS Monthly Newsletter
The latest CNS updates, including events, company information, and patient care developments
The Inside View
Quarterly magazine focused on brain injury research, rehabilitation, and advancements shaping the field
Sign-up for one or both to stay connected with brain injury news and recovery





